When Lawrence and Penny Higgins of Fairfield, Maine, first discovered in 2020 that top ranges of poisonous chemical compounds referred to as PFAS taint their house’s nicely water, they puzzled how their well being would possibly undergo. That they had consumed the water for many years, given it to their pets and cattle, and used it to irrigate their vegetable backyard and fruit timber.
“We wanted to find out just what it’s going to do to us,” Penny Higgins mentioned. They contacted a few medical doctors, however “we were met with a brick wall. Nobody knew anything.”
Worse nonetheless, she added, they “really didn’t want to hear about it.”
Many clinicians stay unaware of the well being dangers linked to PFAS, quick for perfluoroalkyl and polyfluoroalkyl substances, regardless of rising medical and public consciousness of the chemical compounds and their toxicity. PFAS can have an effect on almost each organ system and linger in our bodies for many years, elevating dangers of most cancers, immune deficiencies, and being pregnant issues.
These “forever chemicals” have been extensively used for the reason that Nineteen Fifties in merchandise together with cosmetics, cookware, clothes, carpeting, meals packaging, and firefighting foam. Researchers say they permeate water programs and soils nationwide, with a federal research estimating that a minimum of 45% of U.S. faucet water is contaminated. PFAS will be detected within the blood of almost all People, in response to the Facilities for Illness Management and Prevention.
Maine was among the many first states to start intensive water and soil testing and to attempt to restrict additional public publicity to PFAS by coverage motion, after discovering that farms and residences — just like the Higgins’ property — had been contaminated by land-spreading of wastewater sludge containing PFAS. Publicity may also be excessive for folks residing close to army bases, hearth coaching areas, landfills, or manufacturing amenities.
In areas the place testing reveals PFAS scorching spots, medical suppliers will be caught flat-footed and sufferers left adrift.
Rachel Criswell, a household observe physician and environmental well being researcher, is working to vary that. She was finishing her residency in Central Maine across the time that the Higginses and others there started discovering the extent of the contamination. Her medical coaching at Columbia College included greater than a yr in Norway researching the consequences of PFAS and different chemical compounds on maternal and toddler well being.
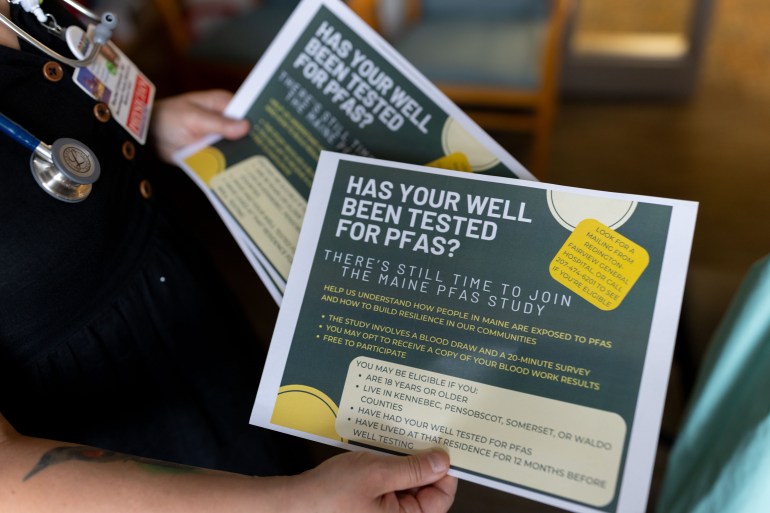
When sufferers started asking about PFAS, Criswell and the state toxicologist provided major care suppliers lunchtime displays on the way to reply. Since then, she has fielded frequent PFAS questions from medical doctors and sufferers all through the state.
Even educated suppliers can discover it difficult to remain present given quickly evolving scientific info and few established protocols. “The work I do is exhausting and time-consuming and sometimes frustrating,” Criswell mentioned, “but it’s exactly what I should be doing.”
Phil Brown, a Northeastern College sociology professor and a co-director of the PFAS Challenge Lab, mentioned the medical neighborhood “doesn’t know a lot about occupational and environmental health,” including that “it’s a very minimal part of the medical school curriculum” and persevering with training.
Courtney Carignan, an environmental epidemiologist at Michigan State College, mentioned studying of PFAS publicity, whether or not from their ingesting water or occupational sources, “is a sensitive and upsetting situation for people” and “it’s helpful if their doctors can take it seriously.”
Medical steering regarding PFAS improved after the Nationwide Academies of Sciences, Engineering, and Drugs launched a report on PFAS in 2022. It discovered sturdy proof associating PFAS with kidney most cancers, excessive ldl cholesterol, decreased start weights, and decrease antibody responses to vaccines, and a few proof linking PFAS to breast and testicular most cancers, ulcerative colitis, thyroid and liver dysfunction, and pregnancy-induced hypertension.
That steering “revolutionized my practice,” Criswell mentioned. “Instead of being this hand-wavey thing where we don’t know how to apply the research, it brought a degree of concreteness to PFAS exposure that was kind of missing before.”
The nationwide academies affirmed what Criswell had already been recommending: Docs ought to order blood exams for sufferers with identified PFAS exposures.
Testing for PFAS in blood — and for associated medical situations if wanted — can assist ease sufferers’ anxiousness.
“There isn’t a day that goes by,” Lawrence Higgins mentioned, “that we don’t think and wonder when our bodies are going to shut down on us.”



‘Devastating but Incredibly Helpful’
After discovering out in 2021 that his household was uncovered to PFAS by sludge unfold on their Unity, Maine, farm a long time earlier, Adam Nordell found that “it was exceedingly difficult” to get examined. “Our family doctor had not heard of PFAS and didn’t know what the test was,” he mentioned. A lab technician wanted teaching from an outdoor skilled to supply the check. The lab analyzing the samples had a backlog that left the household ready three months.
“The results were devastating but incredibly helpful,” Nordell mentioned. Their blood serum ranges for PFAS have been at roughly the 99th percentile nationally, far greater than their well-water ranges would have predicted — indicating that further publicity was in all probability coming from different sources reminiscent of soil contact, mud, and meals.
Blood ranges of PFAS between 2 and 20 nanograms per milliliter could also be problematic, the nationwide academies reported. In extremely contaminated settings, blood ranges can run upward of 150 instances the 20-ng/mL threat threshold.
Nordell and his household had been planning to stay on the farm and develop crops much less affected by PFAS, however the check outcomes persuaded them to depart. “Knowledge is power,” Nordell mentioned, and having the blood information “gave us agency.”
The nationwide academies’ steering paved the way in which for extra clinicians to order PFAS blood exams. The fee, usually $400 to $600, will be prohibitive if not picked up by insurance coverage, and never all insurers cowl the testing. Deductibles and copays may also restrict sufferers’ capability to get examined. More cost effective finger-prick exams, administered at house, seem to seize among the extra generally discovered PFAS as precisely as blood serum exams, Carignan and colleagues discovered.
Maine legislators lately handed, with overwhelming help, a invoice — modeled after one in New Hampshire — that might require insurers to contemplate PFAS blood testing a part of preventive care, nevertheless it was carried over to the following legislative session.
“In my mind, it’s a no-brainer that the PFAS blood serum test should be universally offered — at no cost to the patient,” mentioned Nordell, who now works as a marketing campaign supervisor for the nonprofit Defend Our Well being. Early screening for the ailments related to PFAS, he mentioned, is “a humane policy that’s in the best interests of everyone involved” — sufferers, suppliers, and insurance coverage corporations.
Criswell tells colleagues in household observe that they’ll view elevated PFAS blood ranges as a threat issue, akin to smoking. “What’s challenging as a primary care doctor is the nitty-gritty” of the testing and screening logistics, she mentioned.
In trainings, she shares a handout summarizing the nationwide academies’ steering — together with related heath situations, blood testing, scientific follow-up, and publicity discount — to which she has added particulars about lab check order codes, insurance coverage prices and protection, and water filtration.
Criswell served on an advisory committee tasked with allocating $60 million in state funds to deal with PFAS contamination from previous sludge-spreading in Maine. The group beneficial that labs analyzing PFAS blood exams ought to report the outcomes to state public well being authorities.
That change, slated to take impact this summer season, will enable Maine well being officers to observe up with individuals who have excessive PFAS blood ranges to higher decide potential sources and to share info on well being dangers and medical screening. As with many earlier PFAS insurance policies, Maine is among the many first states to undertake this measure.
Screening for PFAS is falling quick in lots of locations nationwide, mentioned Kyle Horton, an internist in Wilmington, North Carolina, and founding father of the nonprofit On Your Facet Well being. She estimates that solely about 1 in 100 folks dealing with excessive PFAS publicity are getting enough medical steering.
Even in her extremely contaminated neighborhood, “I’m not aware of anyone who is routinely screening or discussing PFAS mitigation with their patients,” Horton mentioned. Information of native PFAS threats, she added, “hasn’t translated over to folks managing patients differently or trying to get through to that next phase of medical monitoring.”


Sufferers as Advocates
In closely affected communities — together with in Michigan, Maine, and Massachusetts — sufferers are pushing the medical subject to higher perceive PFAS.
Extra medical doctors are talking out as nicely. Testifying earlier than a Maine legislative committee this yr in help of a invoice that might restrict occupational PFAS publicity, Criswell mentioned, “We, as physicians, who are sworn to protect the health of our patients, must pay attention to the underlying causes of the illnesses we treat and stand up for policy solutions that reduce these causes.”
Even the place coverage modifications are instituted, the bodily and psychological toll of “forever chemicals” will prolong far into the long run. Criswell and different Maine medical doctors have noticed power stress amongst sufferers.
Nordell, the previous farmer, described his household’s contamination as “deeply, deeply jarring,” an ordeal that has at instances left him “unmoored from a sense of security.”
To evaluate the psychological well being penalties of PFAS publicity in rural residents, Criswell and Abby Fleisch, a pediatric endocrinologist on the MaineHealth Institute for Analysis, teamed up on a research. In its first section, winding up this summer season, they collected blood samples and detailed life-style info from 147 folks.
Nordell, the Higginses, and different Central Maine residents sit on an advisory board for the research, a step Criswell mentioned was essential to making sure that their analysis helps these most affected by PFAS.
“The urgency from the community is really needed,” she mentioned. “I don’t think I would be as fired up if my patients weren’t such good advocates.”
Criswell has confronted what she calls “cognitive dissonance,” caught between the deliberate tempo of peer-reviewed medical analysis and the quick wants of sufferers wanting to decrease their PFAS physique burden. Initially she thought of inviting residents to take part in a scientific trial to check therapies which can be thought of secure and should assist cut back PFAS ranges within the physique, reminiscent of high-fiber diets and a drug designed to scale back ldl cholesterol referred to as cholestyramine. However the scientific trial course of might take years.
Criswell and Fleisch are as a substitute planning to supply a case collection on PFAS blood-level modifications in sufferers taking cholestyramine. “We can validate the research results and share those,” Criswell mentioned, probably serving to different sufferers.
Alan Ducatman, an internist and occupational doctor who helped design the largest PFAS cohort research thus far, mentioned suppliers ought to convey that “there is no risk-benefit analysis” for any of the present therapies, though they’re usually well-known and low-risk.
“Some people want to be treated, and they should be allowed to be treated,” he mentioned, as a result of figuring out they’ve excessive PFAS ranges of their our bodies “preys on them.”