ANCHORAGE — There was one bed coming available in the intensive care unit in Alaska’s largest hospital.
It was the middle of the night, and the hospital, Providence Alaska Medical Center in Anchorage, had been hit with a deluge of coronavirus patients. Doctors now had a choice to make: Several more patients at the hospital, most of them with Covid-19, were in line to take that last I.C.U. spot. But there was also someone from one of the state’s isolated rural communities who needed to be flown in for emergency surgery.
Who should get the final bed?
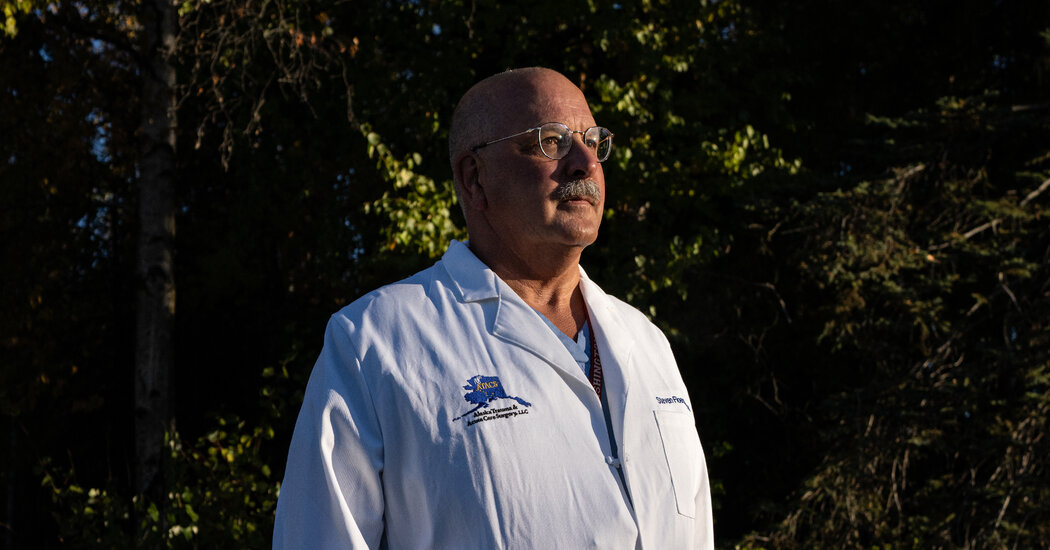
Dr. Steven Floerchinger gathered with his colleagues for an agonizing discussion. They had a better chance of saving one of the patients in the emergency room, they determined. The other person would have to wait.
That patient died.
“This is gut-wrenching, and I never thought I’d see it,” said Dr. Floerchinger, who has been in practice for 30 years. “We are taxed to a point of making decisions of who will and who will not live.”
Since that night, more grim choices have had to be made as Alaska confronts what is currently the nation’s worst coronavirus outbreak. Nearly two years after the virus began circulating in the United States, some of the scenes here on the country’s northern frontier echo the darkest early days of the pandemic: testing supplies are depleted, patients are being treated in hallways and doctors are rationing oxygen. With emergency rooms overwhelmed, the governor has asked hundreds of medical workers to fly in from around the country to help.
Through much of the pandemic, Alaska’s natural isolation had shielded the state, with the early months defined by strict testing protocols for people arriving from the outside. Many villages locked down. When vaccines arrived, there was a legion of planes, ferries and sleds to bring doses to far-flung communities. The state has maintained some of the lowest death numbers in the country.
But with some pockets of the state wary of taking vaccines — only about half the state’s residents are fully vaccinated — and Gov. Mike Dunleavy resisting restrictions to curtail the virus, the state’s isolation has become a growing liability as the Delta variant sweeps through. The state’s surge has continued even as the virus has receded nationwide, with new daily cases down by about a third and hospitalizations by about a quarter since Sept. 1.
Much of the nation’s hospital system has been stressed, but overloaded facilities in the lower 48 states have had more flexibility to transfer patients to neighboring cities or other states. In Anchorage, most of the help is 1,500 miles away in Seattle, and hospitals in the Pacific Northwest have been challenged by their own disastrous virus outbreak.
“When your hospitals are full, you can’t just put them into an ambulance and take them to another town,” Senator Lisa Murkowski said of Alaskan patients in a floor speech to Congress on Friday. She described her own trip to an emergency room in Fairbanks, where a loved one needed help for a non-Covid problem. They were told that critical care beds were full and that they might have to fly to Seattle.
Doctors and nurses have started speaking out in meetings, urging the public to take the virus more seriously, but they have repeatedly encountered hostility.
When the Anchorage Assembly considered a mask mandate last week, some of the doctors who came to speak were jeered at. “Do you use ivermectin?” someone in the crowd shouted, referring to a deworming medicine that has been touted as a Covid-19 treatment on social media even as the Food and Drug Administration has warned people against taking it.
As a group of doctors left the meeting, one person followed them outside, heckling. “You guys have sold out and are liars,” he shouted. Others outside holding signs — “Liberty or Tyranny,” one of them said — also mocked the physicians.
Dr. Leslie Gonsette, an internal medicine hospitalist who often works at Providence Alaska Medical Center, said some of her colleagues had debated whether to even go to the meeting.
“There was an element of caution and worry for our safety,” she said. But in the end, she added, they concluded they had an obligation to tell people about the calamitous scenes playing out at hospitals.
At another meeting of the Assembly the following night, one person was arrested on a charge of disorderly conduct and found to be carrying a concealed weapon. Many people in the audience wore a yellow Star of David, likening the proposed mask mandate to the Holocaust, which led other speakers to express outrage. Mayor Dave Bronson, who has vigorously opposed a mask mandate, argued that it was appropriate to “borrow” the symbol and then later apologized for his remarks.
The debate was scheduled to resume for a fourth day on Monday.
Doctors at Providence, which has now put into place “crisis standards of care” that provide legal clearance for the challenging process of rationing health care, said the process had been traumatic. They have been consulting an ethicist and a triage team. Few have experience navigating such difficult ethical terrain.
The patient who died after being denied emergency surgery was not the only one to undergo a triage choice. In one case, two patients needed continuous dialysis but only one machine was available. Doctors placed one patient on the machine and then switched it to the other. The first patient then died.
Patients with Covid-19, which often results in serious damage to kidneys, have often monopolized dialysis resources, doctors said. When there were not enough machines available at Providence, everyone on dialysis was a Covid-19 patient.
In another case, described by the hospital’s chief medical officer, Dr. Michael Bernstein, a patient with both Covid-19 and extensive cancer was on the verge of needing a ventilator. But with so many patients needing such intense care, that patient was not given life support, and died.
The “crisis standards of care” generally are intended to prioritize the patients most likely to survive. Many states have discussed and approved crisis care guidelines during the pandemic, but few have formally carried them out statewide. Alaska has done so.
Dr. Bernstein said that the triage team had to make rationing decisions in about 10 cases, and that the hospital had also been forced to postpone care in other ways. Twenty-nine cardiac patients have had operations postponed, and the hospital has refused to accept transfer requests for 21 patients.
“This morning, the I.C.U. was completely full, and we had four patients in the emergency room that needed intensive care,” he said.
The struggle is spreading beyond Anchorage. On Wednesday, the Yukon-Kuskokwim Health Corporation in Bethel announced that it, too, had turned to crisis standards of care. “We are now in a position of making these difficult decisions on a daily basis,” the hospital’s chief of staff, Dr. Ellen Hodges, said.
On Saturday, the state said it had activated crisis standards for 20 health care facilities, covering larger cities such as Anchorage, Fairbanks and Juneau, along with smaller ones such as Cordova, Dillingham and Kotzebue.
At the Providence hospital in Valdez, high-need patients who would otherwise transfer to Anchorage are staying put, and there is so much demand for oxygen that the hospital has had to limit the amount each person receives. While patients would normally be kept at oxygen saturation levels of 93 percent, that has now dropped to 90 percent.
Dr. Anne Zink is Alaska’s chief medical officer, helping lead the state’s pandemic response, but she also works as a physician in the emergency room at Mat-Su Regional Medical Center, northeast of Anchorage — a region with some of the state’s lowest vaccination rates and highest hospitalization rates.
Dr. Zink said she had been examining patients in the waiting room and caring for them in hallways. One day, with not even stretchers available, she found herself sitting on the floor to stitch a foot laceration.
“Our goal has always been to avoid having systems overwhelmed,” Dr. Zink said. “And right now we have systems overwhelmed.”
Governor Dunleavy has avoided ordering a statewide mask mandate or other restrictions during the latest surge, saying such requirements should be decided locally in a vast state where some communities have had few or no cases. A draft statewide mask mandate had been drawn up early in the pandemic, Dr. Zink said, but it was never put into place.
With each Covid-19 patient, Dr. Zink said, she wonders if there was more she could have done, something she could have said, to convince more people to get vaccinated or take precautions.
She became a household name at the start of the pandemic, when she gave video briefings to the public from a heated yurt behind her family’s home. In many corners of the state, she has been widely praised. On a recent day, while talking with a reporter at an Anchorage park, a couple walking their dog recognized Dr. Zink and waved. “We are fans,” the man called out.
But Dr. Zink is spending time trying to reach people who are not fans. She has been appearing on conservative talk radio, answering questions and trying to ease fears about the vaccines.
While some people have made up their minds, Dr. Zink said, she still regularly finds others making the decision to get vaccinated. A state survey, she said, found that 60 percent of unvaccinated people are open to it. In trying to encourage people to consider vaccines, she often uses references to moose hunting and berry foraging and all the ways that Alaskans are used to taking care of themselves and one another.
“Just like when we go out in a storm, we layer up,” she said.
“We do multiple things together: We change our snow tires and we wear a jacket and we wear a hat,” she said. “So make sure you’re vaccinated and wear a mask and keep your distance. We know how to do this.”